Hidden in Plain Brain: AI Finds Tiny Lesions in Children’s Epilepsy — A Breakthrough That Could Change Their Futures
An artificial intelligence tool trained to read brain scans is helping doctors spot tiny, blueberry-sized brain malformations in children with epilepsy — lesions that are often missed on standard MRI. Structural abnormalities cause about three in ten epilepsy cases, and many kids who could benefit from surgery are never considered because the lesions hide in plain sight. Researchers say this AI could help families access potentially life-changing surgery sooner, offering a new thread of hope where none seemed possible.
In This Article:
Most Brain Lesions Are Invisible on MRI, Especially the Smallest Ones
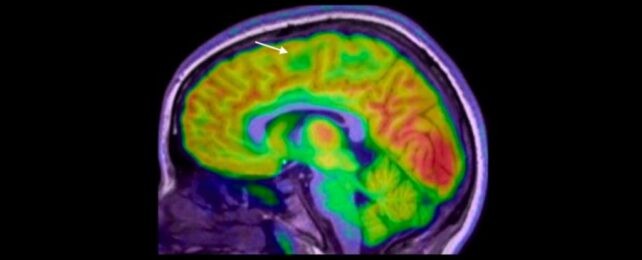
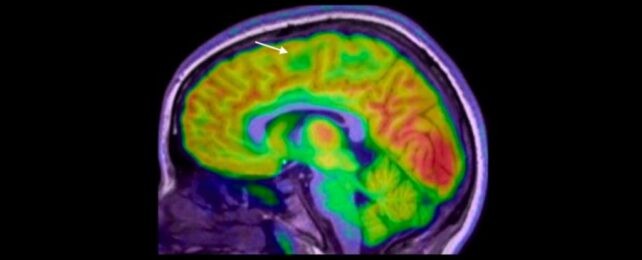
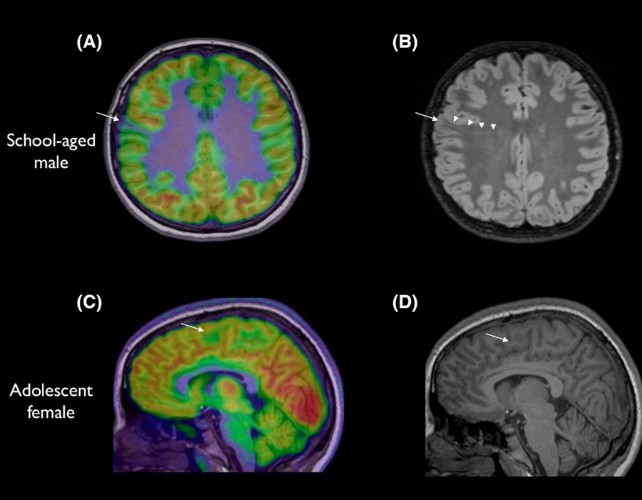
Tiny brain lesions can escape detection on MRI, particularly those tucked at the bottom of a brain fold. In the study, 80% of the children had prior MRI results that were normal, suggesting many surgical candidates were overlooked before artificial intelligence was involved. The scale and subtlety of these abnormalities mean a missed diagnosis can delay life-changing treatment.
AI as a Clinical Detective: The Melbourne Study
Led by paediatric neurologist Emma Macdonald-Laurs at the Royal Children’s Hospital in Melbourne, the team trained an AI tool on pediatric brain images to detect lesions the size of a blueberry or smaller. When the AI analyzed both MRI and PET scans, its performance reached 94% in one test group and 91% in another. Of 17 children in the first group, 12 had surgery to remove their brain lesions, and 11 are now seizure-free. The researchers plan to test the detector in more real-life hospital settings with undiagnosed patients.
Real-Life Impact, Costs, and Cautions
Epilepsy affects about one in 200 children, and about a third of cases are drug-resistant. Experts call these results exciting and a strong proof of concept. A related study from King’s College London using AI on MRI data alone spotted 64% of epilepsy-linked brain lesions missed by radiologists. PET imaging can add value, but it is expensive, less widely available, and involves radiation. The AI tool is not meant to replace radiologists or doctors; it acts as a detective to help piece together clues more quickly.
A Path Forward: Hope, Limits, and What Families Should Know
This work points toward a hopeful future where children with epilepsy access targeted surgery faster and more reliably. The next steps involve validating the detector in more real‑world hospital settings and with new, undiagnosed patients. Families should discuss imaging choices with clinicians, considering both the potential benefits and the costs and radiation associated with PET. If validated broadly, many children could gain seizure freedom and a markedly improved quality of life.